Years ago I worked as an assistant for two neuropsychologists, essentially doing all the face-to-face testing. Usually, this meant 4 to 6 hours crammed into a small stuffy office conducting various cognitive, memory, and intelligence assessments.
3 Important Lessons I Learned:
Although watching patients attempt to stick square objects in round holes had its moments, the lessons I learned about brain functioning have been very influential in my work with those who struggle with addiction.
Lesson #1: It’s not intelligence that matters so much as the level of emotional development
I will never forget a couple who were in the process of divorce and both required by the court to submit to neuropsychological evaluations – something to do with custody issues of their children. The husband went first and scored so high I believe he was in the range of genius – it was the highest IQ score I had ever seen in my two years of doing testing.
The next day his wife came in and I was  unprepared for her IQ score being half of his! In fact, it was clear she had some learning and developmental disabilities. I immediately began to wonder how these two people with drastically different levels of intellect could remain married for over a dozen years.
unprepared for her IQ score being half of his! In fact, it was clear she had some learning and developmental disabilities. I immediately began to wonder how these two people with drastically different levels of intellect could remain married for over a dozen years.
Upon further reflection, I realized that intellect is not the glue that attracts or holds people together, it’s their level of emotional development.
I have wrote about this in a Stanley Greenspan blog post, but continue to bring it up because it points to the absolute necessity of helping those who struggle with addiction developmentally catch-up from the emotional age at which they are stuck.
There are some really smart people that get caught up in addiction, and often they can be among the hardest to treat because they believe they can think their way out of the problem. But you cannot “think” your way to a higher level of emotional functioning.
Lesson #2: The brain needs time following detoxification to heal before it can absorb, process, and benefit from treatment
Advances in neuroimaging have helped establish addiction as a brain disease. The slide on the right shows that 10 days post cocaine use, an abuser’s brain is still very far off from normal baseline functioning (top). 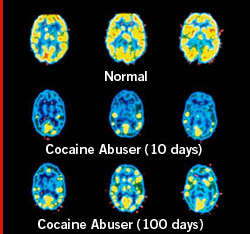 Even more illuminating is the degree to which brain functioning is still impaired 100 days post last use! We see similar profiles for other drugs of abuse including alcohol, and behavioral addictions.
Even more illuminating is the degree to which brain functioning is still impaired 100 days post last use! We see similar profiles for other drugs of abuse including alcohol, and behavioral addictions.
Because neuropsych testing can provide a window into brain functioning, we can use such testing to help us understand how long it takes for the brain to heal to a point at which it is capable of learning, processing, and remembering new information – information such as how to manage addiction over time. Researchers are now doing a battery of neuropsych tests on patients following detox to determine optimal times to begin treatment.
What is clear, is that our current system is set-up to have a person who has completed detoxification immediately enter a residential program. About 1-2 months later – about the time they are being discharged from treatment – is really the time when their brain is ready to benefit from treatment.
I find it sad that significant sums of money are invested in residential programs when science is helping us understand that for treatment to be beneficial a person must not only detox, but also wait a month or two (or even longer, depending on the drug and time used) before engaging in any significant treatment. This of course brings us the messy question of what should a person do between detox and treatment? I welcome your suggestions…
Lesson #3: Neuropsychological assessments can be critical for understanding how to proceed with addiction treatment
While working as a counselor at a community-based addiction treatment program, I encountered a number of patients who suffered from Traumatic Brain Injury (TBI). Usually, the TBI would come up in the evaluation, or it would become apparent when I did a mini-mental status exam.
Today, over 5 million people live with a disability caused from a brain injury, and approximately 70% of those in rehabilitation have a current or past diagnosis of substance abuse.
When I first began encountering addicted TBI patients as an intern, I treated them similar to other patients. I did individual therapy, put them in groups, and proceeded to educate them about ways to deal with their addiction. But over time I realized my outcomes were very poor.
Many dropped out of treatment, others continued but were incapable of remembering what they had learned or how to apply it to their life. Relapse rates were significant. Then I discovered our medical psychology department at the hospital and began referring addicted TBI patients for neuropsychological exams. The reports I got back were invaluable in helping me completely restructure treatment.
Like children, the trick was understanding what they could comprehend and how best to teach them what they needed to learn. I got a blackboard for my office and begin drawing pictures to represent ideas I wanted to get across.
I went slow, paid attention to patients different learning styles, and adapted my treatment approach to the diverse ways in which their brain processed information.
And as you might suspect, my outcomes improved. Utilizing the knowledge from neuropsych assessments, I believe, can make all the difference in the world when working with patients with TBI.
I just watched a powerful documentary on Hulu about a woman’s struggle with addiction and wanted to share. Hearing her struggle just reaffirmed the fact that addiction is a disease of the brain and why for many it seems physiologically impossible not to relapse again and again.
http://www.hulu.com/watch/62675/cracked-not-broken
What should we do with a person between detox and treatment?
The first thing that we should do is recognize that an individual’s environment will contain countless relapse triggers. They will be surrounded by images and other stimuli that are impossible to remove. The urge to use after being exposed to a trigger may be very great.
It seems like one way of tackling this problem is coming up with plans for individuals BEFORE they start rehab for how they will react to these triggers. Admitting to a client that they will be tempted, that they will not always be consciously aware of the trigger but will feel the urge to use just as strongly, and knowing what to do when that happens.
Strengthen current resources. Recognize all the different relationships in an individual’s life that can be utilized to help deter use. Recognizing that some of the relationships that can be helpful can also be triggers, and knowing how these two parts of a relationship need to work together (example: Your mother always yells at you to get a job and it makes you want to drink, but once you are sober you need your mother’s support to stay sober).
This is not a simple solution. Relationships are complex. Problems cannot be solved over night. A single person can fill more than one role in an individual’s life (example: one person may be coworker, motivator, drinking buddy and more). Knowing how relationship patterns encourage relapse but can be changed to help abstinence is a practical first step to utilizing the support system. It encourages clients to use the systems already in place to help promote change.
In evaluating an individual with TBI, it will also be important to understand any neurochemical changes that may have occurred as the result of the trauma to the brain. TBI can result in drastic changes in both structure and function of the brain. This condition is called Organic Brain Syndrome (OBS) and has many causes including concussion trauma, intercranial bleeding from an aneurysm, bleeding into the space surrounding the brain, pressure on the brain from blood clotting, alcohol and/or drug withdrawal, and the long-term effects of alcohol or drug abuse. OBS does not include psychiatric disorders but can include seizure disorders.
The effect of TBI on the brain has been likened to an electrical storm of brain activity that is not within the individual’s control. As part of the treatment for OBS, medications may be needed to reduce aggressive behaviors that can occur with some of the conditions. Unfortunately, many of these medications can be used excessively or in combination with other substances to achieve heightened effects.
Added to the neurochemical changes and the medications is the psychosocial impact of living life as a person with a TBI. There are difficulties with planning, poor memory issues, emotional control problems, depression, anxiety, changes in family roles, and changes in work relationships. Because the damage is physical, individuals can perceive themselves as never having a ‘real’ life again, as having little value, as being ‘less’ than they were, as not worthy of caring relationships. With such self-defeating aspects practically built into a TBI condition, it is easy to see how ongoing brief interventions could be critical to helping individuals with TBI avoid addiction or at least, minimize the risk.
Awareness of this correlation is particularly important now because TBI is the number one injury for servicemembers coming back from the war.
Kelly – good call! Watched it and blogged about it.
The comments on the differences in the IQ levels of the couple going through a divorce should serve as a wake-up call to all therapists. It can be easy to believe that individuals with a higher education will be better able to avoid addictions but mere knowledge isn’t always power.
Having worked in a health care setting most of my life, I have consistently seen doctors, nurses, and therapists that are overweight, smoke, drink excessively, gamble, and take drugs. These are all highly trained, highly educated people working in the field of health and yet they are no more immune to the hijacking of the mind than the average individual.
It is necessary to ascertain the level of the client’s emotional development to have a better chance of a successful intervention. If the level of treatment is targeted at the intellect rather than the emotional level, then what we as counselors are ‘pitching’, our clients won’t be ‘catching.’
The idea presented in this blog that the level of emotional development is more important factor that intelligence (IQ) in developing relationships can be seen with the students that I work with who are in the autism spectrum. Most of the students fall in the category of Asperger syndrome, characterized by low nonverbal communication skills, limited empathy and physically awkwardness. These students have a disorder that can is demonstrated in their emotional development. Many of the students I work with who are in this spectrum are getting straight A’s but do not have very many friends. If they do have a few friends their friends also have lower emotional abilities.
The most poignant example was when two students who are friends and who both are in the autism spectrum were trying to figure out how to talk to girls. The closing of the conversation was when one boy said, “Why would you want to talk to girls anyway?” These young men, who are about to graduate from high school are totally successful academically but will need a lot of continued help to be successful in their relationships with others.
I have an husband and I am attempting to keep out of the house, that for years his alcoholism has driven me crazy, trying to reach him was an impossible task.
I have 3 teenagers whom he gets along very well with and they all gang up on me when I lay down the law of control in my home, in which he does not reside but does visit, which has caused a great deal of conflict. He acts and thinks like my teenagers, I have noted that he is the teenager with the car a lot of money and power because he is 40.
I try to only observe now instead of trying to communicate with him. I am relieved to know that my children will grow and mature but he is done maturing, because his father had him drinking at 3 and used to beat the snot out of him, his brothers and his mom. If I talk to him like my teenage son and let back talk slide it is amazing how much better we get along.
I don’t wish to sound like I am demoralizing him that is not my intention, it was just such a relief to have a greater understanding of his brain and know that I am not crazy.
It is very difficult to be in a home with 4 teenagers and 1 with a lot of power and pull, it can be very tiring.
Susan, glad the post helped. Sorry to hear about the struggles with your husband and his drinking. You may benefit from reading: http://addictionmanagement.org/loved-one-friend/
J
It is very disturbing that treatment is being administered before the brain is able to effectively absorb and learn. This knowledge will hopefully lead to insurance coverage being expanded to pay for longer term treatment programs. As for what to do between detox and treatment, I think you still need to provide treatment. To not treat people post detox and to have them out on their own would lead to staggering levels of relapse. A change in the treatment iteself may be the answer. I think the treatment, in the period before the brain has been able to recover, should be focused on more general health areas such as improved nutrition, promoting healthy activities and exercise, and creating a healthy recovery environment. Maybe this early treatment would not be as intensive but it would still provide a regular structure that the individual could count on and facilitate a healthy lifestyle change. This structure would be in place once the individual’s neurological health was improved to allow for the maximum potential effectiveness of treatment.
I am intrigued with the idea of being developmentally behind emotionally despite intellectual capacity. I would also think that it would be impossible to maintain a relationship with someone who possesses a staggeringly different level of intellect. But I too have encountered people in life who are just not emotionally advanced despite their knowledge. It would seem imperative that counselors become aware of this topic and be able to note the developmental level their patients are at. I don’t think that gets noticed as often as it should and as a result patients suffer. That being said, the treatment system currently doesn’t do justice to these needs either. It seems there has to be some way to transmit this information to various platforms in order to ensure the system changes.
Frankly, it’s not surprising to me at all that the science is being ignored in treatment. If we were to acknowledge the scientific findings around addiction, we would have to change our ideas about addiction being a choice the person makes. What is exciting, however, is that we can only ignore science for so long, and then the cognitive dissonance becomes too loud to ignore. The question of what to do to help a person while they are de-toxing and regaining brain function is a tough one. Even with science on our side, there is still a great deal of uncertainty about what the best practice could be. Obviously, you don’t want to send the person back to the environment that supported their use in the first place when they are so freshly sober and relatively vulnerable to relapse. What then is the alternative? I keep getting pictures of summer camps in my head. This is impractical and expensive. Newly sober people still need support and help from helping professionals. Perhaps waiting to do skill building is appropriate, but people still need to learn how to build relationships all through the time that the brain is recovering. I think this idea kind of ties in with the developmental age and emotional intelligence. Perhaps as the brain recovers, the client is in a special position to heal some of the developmental issues in his or her life.
My response is that I had never really considered the emotional development of the injured and damaged brain prior to this reading. It makes sense that after the addiction begins that the brain does not develop very much because it is too busy becomming numb from the drug or alcohol abuse.
From my personal perspective, my mind just “woke up” after several months of abstinence from alcohol. After my mind had healed, at least to some extent, my mind became very active. It was almost as if I had been taking stimulants but I was alive and full of thoughts that were good and positive and healthy.
Thank you for this post. I think it is so important to recognize that the brain takes times to develop new pathways, and though neuroplasticity is possible, it takes a lot of work. Neuroscience is proving more and more today that the emotional development is in fact the most important factor in development. First, in prenatal development, then looking at the first eight months of life, and continuing on by looking at the environment a child was exposed to. In an interpersonal neurobiology class I am taking, we often look at the development of the brain up until the age of two. This environment is so important in looking at emotional development. Teens using substances are missing out on often huge chunks of what could be emotional development, but “numb” the pains or pleasures that they are experiencing. If a teen or young adult misuses substances for longer than ten years, recovery becomes even more difficult to attain. So, I am really glad that you focused on the emotional development, as I think this may be the key to connecting with others.
I also really appreciated what you shared about the brain after a year of recovery. I have read that after a year of recovery, because the brain has been learning new ways to function, respond, attach, react, etc. and new pathways are forming, an individual will be able to handle situations with more clarity and self-control. During the time between intervention and this year mark, I think encouraging a person to develop new behaviors, people, places, and things are so important. As someone else eluded to, many of these aspects in a person’s life will be triggering. The key is to create a life that has fewer triggering situations, so that the person can slowly learn to calm their limbic brain in a variety of situations, and eventually learn new behaviors.
Sara, I really like your previous posting about what to do during de-tox. Idyllic mental pictures of summer camp are hard to supress. I agree that this type of de-tox setting would be both impractical and expensive. Which makes me wonder, how could a summer camp model be made more realistic for detox?
Removing patients from the environment that triggers and perpetuates their addiction seems invaluable. In the first few days and weeks of detox, when a person is so susceptible to relapse and unable to fully benefit from treatment, I wonder if providing a safe environment, healthy food, and some sort of structure for meaningful work and creativity is the most therapeutic thing do be done.
In my experience, one of the most beautiful things about summer camp is the depth of the relationships that are built there. The bonds that are forged at camp aren’t based on similar interest, but on shared experience. Providing opportunities for patients to build relationships with one another apart from their similar interest in addictive behaviors, would be a powerful tool for improving self-efficacy.
Obviously, our system of immediate residential is not a model well supported by the current science but what alternatives exist? I like Sara’s summer camp idea but she admits herself that it is impractical and expensive. Unless we can find financial support for longer term residential care we seem to have little options.
Could we possibly postpone residential treatment, for one or two months after detox as the science suggests and fill that time with out-patient treatment to reduce relapse? It seems impractical because of the high rates of relapse likely to occur but if patients were monitored and attended counseling during this out-patient period, could the relapse rate be reduced enough to improve the overall efficacy of the addiction treatment system? So, instead of the current detox, to residential, to intensive outpatient treatment that tapers off, the system might start you in detox, move you to intensive outpatient, then residential and finally light out patient counseling. It seems doubtful that this system would work, but not impossible. Until there is financial support for longer term residential programs, other options, however unlikely sounding should be considered.
It makes sense to utilize neuropsychological assessments in the treatment of addicts with TBI. As with children, the point shouldn’t be to talk down to them, but to meet them where they are developmentally. This also ties in to emotional development, as tailoring therapy to correspond and relate with the client’s emotional age is important for the emotional resonance of the therapy to take hold. Wherever the client is, in terms of cognitive and emotional abilities, it seems integral that the therapist recognize and honor where that person is coming from.
In regard to asking what people should do in the space between detox and treatment when their brains are healing, I thought of the Michael Moore movie Sicko, in which he profiles a French citizen who rehabilitates on the beach for a couple of months following cancer treatment, all paid for by universal healthcare. It seemed to promote health and healing, and spending a couple of months relaxing in the sun would probably be beneficial to people with addictions. I feel like a lot of people don’t think addicts “deserve a vacation” for being addicts, though, especially if they’ve done some gnarly things in the course of their addiction, or seem amoral in their behavior.
I agree with and can attest to the fact that neuropsychological assessments can be critical for understanding how to proceed with addiction treatment. An example comes in the form of a patient whom I was working with who was engaged in court mandated treatment for multiple DUII offences. This patient had, in fact, engaged in and completed the very same supervision and a similar treatment program 7 years prior to my encounter with him. This individual was perhaps the perfect example of how chronic and persistent addiction has become in that despite years of treatment and intensive supervision, the threat of prison, and the damage he had caused himself and his family, he continued to use, drink, and drive.
His treatment began and ran the course of many others in the very same program. Around the time of his engagement in a relapse prevention psycho-educational group that I was running he relapsed. In the aftermath of his relapse through our sessions it became very clear that he was not learning and processing the materials and concepts presented in his group. A referral for neuropsychological assessment successfully completed changed this patient’s course through treatment. The assessment came complete with suggestions on what modalities of treatment might be most effective and gave the patient, treatment providers, probation officers, and the court a more accurate picture of this patient’s cognitive capacity and the potential impact on treatment outcome expectancy. I’m happy to say, though very guardedly, that this patient successfully completed treatment over one year ago and remains (as reported by his supervising entity) alcohol, drug, and probation violation free.
I just recently read the very long article on development and how we should make certain to look at one’s developmental level in coordination of care. i think about Piaget and how education should be tailored to the childs current development and ability. I also think about a guy I dated, he was a marijuana addict; I tried so hard to “save him from himself,” but realized later that her really was stuck, I remember thinking wow “he’s such a child,” and learning more about addictions now, I realize that he really was. having smoked marijuana for all his life, I can conceptualize now how his brain had affected and why each time I asked him to stop; he couldn’t. In my place of work I don’t see use of science in treatment-why is it that something so real can be avoided? How can you expect to simply detox someone for a month and that be it? All of this is so frustrating….but yet how do we make a change?
I really appreciated the comments made about the difference between intellectual and emotional development. It is such an important distinction. I can think of people who are extremely well educated but are still immature in many ways. Likewise, I can think of people who never even graduated high school who are extremely emotionally developed. I would have to say that in many ways the uneducated, yet emotionally mature individual will most likely end up happier and healthier in their life. Intelligence can only take you so far. It is important to remember these distinctions when working with clients and to not assume an individuals level of education is the same as their ability to interact in a healthy emotional way.
I find this research on the healing of the brain post-addiction to be facsinating. Hopefully with this knowledge our care system can begin to make the neccesary changes. I like the idea of summer camp; it sounds fun, but perhaps not feasible. However, I can imagine some type of sober-living transitional housing that people can live in during the time between detox and treatment where they can live with people who are going through similar struggles and be in an environment that teaches healithier ways of living before actually entering treatment.
In reading this I started to muse on the problems posed by treatment being unable to truly begin until the system is completely purged of the former object of addiction. What is to be done in this gap of time? It truly is difficult to plan around but I think some work can be done. Perhaps in the time before being “purged” coaching, education and such could be a good focus. Insight exploration seems best put off until this gap is over. I imagine support groups and such would be another good route to take. Being around others trying to make the same changes could allow the clinician to create a temporary bridge to treatment proper.
The distinction between emotional and intellectual development is quite interesting. This is something that I have learned about this term in this class another on teaching and learning, and now that I have this knowledge I see it in action in my work with children. Some children just get so worked up and can’t express this in anyway but to cry and throw a fit. Equipped with this knowledge of different developmental levels of children I have seen a drastic improvement in my ability to quell the constant eruptions that occur daily at a child care center.
Taking time to try and talk about what they are feeling and thinking has given some of my children an easier time dealing and thinking about their current issue, it also seems to be helping some of them repeat these reactions over and over, as was likely to occur before.
In essence learning to assess where our client’s emotional and intellectual levels should help give us a better fighting chance at trying to help them enact the changes that brought them to us in the first place.
Be well and joyous!
Luis G.
Emotional development is vital to recovery process in addiction treatment. Intelligence is more static than emotional development. As clinicians it is our duty to work with our patients where they are at intellectually and emotionally. We cater our treatment to an individual’s intellectual level, learning style, life experiences, strengths weaknesses etc. It is our job to assist our clients in developing emotionally to help in both interactions with others as well as the way which one views his or herself. I work with youth with a variety of intellectual levels. I too am surprised at the discrepancy between intellectual and emotional functioning. Most of the young adults with higher emotional intelligence have better outcomes in terms interpersonal relationships and success with achieving personal and professional goals. While intelligence may be a strong predictor of success, it does not necessarily measure how one deals with life’s challenges. The fact that many of our client may stuck at the emotional level prior to dependence implies the earlier one started abusing the more work we must do with our clients to foster their emotional development.
All three of these neurological lessons speak volumes to the importance of understanding a client’s developmental level, both emotional and cognitive, and knowing how and when to therapeutically intervene. Without this knowledge, as therapists we will never be able to meet a client where they are at or create the therapeutic alliance that studies show makes a true difference in client change. Fortunately, we already have the technological tools to identify this valuable information, what’s needed now is better access to proper training on how to implement therapeutic interventions at each corresponding level.
To solve the conundrum of what to do with clients during the period between detox and full brain recovery, I believe a system-wide change is needed in the way health care facilities think of addiction treatment plans. One idea might be to assign a specific health care professional to each individual who is just out of detox to act as the individual’s case manager or “sponsor”. This person would be responsible for helping the individual design a safe and healthy environment to live in – one far away from the triggers that could propel them into relapse. This interim “home” would be built from preexisting resources within the individual’s life or those from the community. The case manager would also perform daily check-ins and weekly home visits to ensure that the individual continued to have the proper emotional, physical, and relational supports in place to maintain sobriety until the brain fully healed and effective addiction management treatment could commence. This idea may seem idealistic and cost-prohibitive, but when you consider that more than half of those treated for drug or alcohol abuse return to active use within a year and will most likely need costly treatment again, perhaps this relapse prevention measure would be worth every penny.
“The brain needs time following detoxification to heal before it can absorb, process, and benefit from information discussed in treatment.”
While my lack of confidence in the above statement may stem from my admittedly limited knowledge of the research, I’m not yet convinced that treatment shouldn’t start right after detoxification. Dr. Fitzgerald states that as the brain recovers to normal baseline functioning, it is impaired in its capacities for “learning, processing, and remembering new information”. However, even though the patient’s impairments inhibit their ability to get the most from treatment, this is also a very critical time to provide a lot of support and structure to prevent a relapse, as the drug affected brain must be very susceptible in this physiologically modified state. Our understanding of addiction as a chronic condition would suggest that treatment should not be aborted as the brain returns to normal functioning, as has been the case, but that is not to say treatment shouldn’t be started prior to this return to baseline as well. While the addicted brain my demonstrate shortcomings, it still likely retains some functions and abilities that can be utilized in treatment.
Perhaps the question should be less about when to start and stop treatment, and more about determining the modes of treatment that will be effectively received by the patient at a given time based on discrete levels of recovering functionality. For example, perhaps simplified deliveries of repeated psychoeducational treatment can be beneficial early on as a way to set the stage for more advanced conceptual deliveries later along with trauma work once the brain has recovered the necessary capacities for the treatment to be practical.
I worked with a young teenage boy in an inpatient psychiatric facility who was a perfect example of being very traditionally intelligent but emotionally stunted. This kid had a history of trauma and on the few occasions that he was willing to communicate his bottled up thoughts, it was evident that he used his intelligence to support and rationalize the cold and twisted world that he had experienced. Through his intellect he was able to develop a complex and rigid schema that accounted for the people in his life in a very critical and negative way. However he did not seem to integrate an emotional component into his view of the world, perhaps because emotions were foreign and ambiguous to him. Regardless, his advanced intelligence and restricted emotional development may prove to be a huge hurdle for him, as he was aware of his cognitive capabilities and therefore confident that his view of the world was “right” and “accurate”. In the end I’m worried that he may just use that rigid world view as barrier, limiting his chances of future emotional development.
Since the primary treatment modality for addiction is group therapy, neuropsychological assessments are paramount, in aiding treatment success. One of my favorite in-class stories this term, was regarding Dr. Fitzgerald’s patient who had countlessly been in and out of group treatment. In fact, this client NEVER participated in any individual treatment throughout his disease. Though Dr. F developed a strong rapport with his client, and felt confident they made substantial, collaborative progress, the client consequently relapsed. Post treatment, Dr. F realized he should have worked more specifically, with this client’s developmental constrictions and/or deficits. Neuropsychological testing can help clinicians, more appropriately group patients with others at a similar emotional and cognitive level. Especially in terms of groups, as many different people are receiving the same treatment from 1-2 group leaders. If everyone in the group is not at the same or at least similar developmental level, it certainly will harbor some or all success, and potentially even worsen or perpetuate some underlying issues. Funding is often a barrier to providing clients with optimal care, but as clinicians we should be as astute as possible to identifying such incongruencies and all we can to realign fitting care.
What should a person do following detox and treatment? I wanted to comment how much I’ve enjoyed reading everyone’s creative, responses to this question. I suggested in another post that we implement creative therapies, activities, and workshops following detoxification; in addition, I feel that incorporating a more systemic involvement at this time could also be beneficial. Related to an intervention, this time could be used to emphasize the consequences of the disease on family and loved ones, but also stressing the unconditional love, encouragement, and support of family. Often times family members are enablers and may even be triggers for addictive behavior. Treatment should extend out to the client’s family and train them how to positively interrelate with the addict. Train families to shift the system, under the addict’s feet and make it much less rewarding to use any longer- similar to the Community Reinforcement Approach. Also, while the addict is in treatment, I feel the family should be a consistent, positive, loving and supporting presence throughout the experience, proactively via phone, email, letters, etc. Ultimately addressing at least some of the patient’s therapy with a systems therapy approach could be useful with identifying underlying traumas or relational deficits. Increasing emotional commitment to family and loved ones may increase commitment to healing and self-efficacy.
I wanted to comment on Michael’s comment – I was talking to my friend yesterday who teaches in the Speech Pathology program at PSU and she was saying that there is a very high rate of suicide in adults with autism. She feels that it is a population of people that is often forgotten about. As Michael was saying, people with autism often have a difficult time with social skills, so one can imagine how isolating life could be once someone with Autism leaves high school may no longer have the strong support of the school or their families.
I’m gonna go out on a limb here as to what a person should do between detox and treatment – how about yoga? Yoga can further help detox and support the physical body, and it doesn’t really matter what your emotional maturity level is, one still tends to get something out of it! I know many people who credit yoga with being the main thing that helped them overcome their addiction.
I think the concept of emotional intelligence is very important. I have a friend who is struggling with addiction and emotional problems stemming from early childhood sexual abuse. When she is intoxicated she speaks extremely softly and uses “baby talk.” I used to get very frustrated with her but I think I now realize that she got “stuck” at that early level of emotional development. When sober, if she’s really stressed out she will speak in “baby talk” as well. Unfortunately, she refuses to seek help and continues to believe that she can “think” her way out of addiction. This isn’t working. My hope for her is that she will find the courage to confront the emotions and experiences from her childhood that continue to hold her back and constrict her emotionally.
I had a friend who was a meth addict. She probably checked into five different treatment centers starting at the age of 16. She would get sober for different amounts of time but always eventually relapse and hit the drug harder. At age twenty-eight she started landing in jail for misdemeanor offences. She would be held for about a week at the most, required to complete an addictions package (90 AA or NA meetings, stay out of bars, get a mandatory evaluation, and commit no more crime). The cycle continued over and over for about a year, until one day I got a desperate call from the Columbia County Jail where she had been recently detained. A judge had told her that if she could get somebody with a current license to drive her to a in-patient treatment center, complete treatment without any setbacks he would waive her sentence. If she failed in anyway he would giver her no less than eight months for her latest crime. I agreed to take her to treatment and wished her well. Thirty-three days into a forty-five day treatment program she walked out the center and caught a bus back to Portland where she relapsed and ended up serving eight and half months in jail. After jail she was mandatorily checked into another program and completed it and has been sober since. That was seven years ago. When I asked her what the difference was this time she told me that there was no way she could have utilized the tools of treatment until she had been forced to be sober for six months. It was at this point she felt the emotional and physical cravings finally subsided enough to use treatment. I bring her story up as living evidence to the idea most treatment is completed before effective detox is accomplished. While it is unreasonable to suggest that all addicts hoping to get clean be forcibly locked up in order to complete treatment, couldn’t we use the evidence we have and make detox, even at 120 to 150 days, part of in patient treatment?
I think the power of visually presenting the effects of a drug (or anything reckless) on a persons body is an effective tool in prevention or cessation. I remember driver’s ed class showed a powerpoint presentation of people’s maimed bodies after car crashes involving people not wearing seat belts. The pictures were horrific and needless to say I wore my seat belt after that presentation. I think the same concept applys to these neuropsych scans. If I saw an example of these brain scans during or before my “experimental phase” I would have stopped “experimenting” or maybe never even started. The Oregonian even did an effective before and after presentation with the front page pictorial of “the faces of meth;” seeing is believing.
I liked the reading on Healing Trauma: A Therapists Reflection on What Works because I thought it was relative to how the brain reacts to trauma in comparison with drug use and addiction, but is stimulated by a negative memory while telling and re-experiencing the traumatic event, because it includes the physical experience which has been neglected by verbal therapy alone and your ability to hear and connect with the patients experience allows for validation and “trust”. Great reflection!!
I really like learning about this neuropsych stuff not only because I think that the brain is facinating, but I find it is really validating t to incorporate the objective scientific evidence into therapeutic practice/treatment. I don’t that is done quite enough. However, I think it is important to find a balance because I don’t think this purely science but also an art.
The most interesting thing that I learned is about the need for the brain to repair between detox and treatment. I think that the whole system would improve if the people who ran these programs looked at this research and incorporated it into their programs. I wonder if there has been research further looking what a proper time is to begin treatment.
I think that the time between treatment could be used to make sure that clients are safe and have their essentials taken care of (while in treatment and after). Also it would be great to incorporate yoga or other relaxation techniques.
Katie, I agree and definitely think that anytime is a good time to incorporate relaxation techniques, a good diet, and exercise (but, the sooner the better). This is the basis of a healthy life-style, which I believe is key to addiction recovery and addiction avoidance.
In my graduate studies I am researching the need of emotional intelligence in addiction recovery, and how such intelligence can be obtained and/or increased. For example, I think the companionship of animals has the potential to increase emotional intelligence and thus help with addiction recovery. Incorporating information from Dr. Fitzgerald on neuropsychology of addiction will help. I especially like the statement that emotional development is more important than intelligence. I would consider that the increase in emotional development increases emotional intelligence.
Wouldn’t you say that there are things that a person can do during detox, between detox and treatment, during treatment, and even (or maybe especially) after treatment that has the potential to continue to increase emotional development and thus help in recovery? Things that are helpful and maybe necessary in changing one’s life-style, such as education and practice in healthy eating, exercise, effective sleep, relaxation, time and stress management, knowing and avoiding one’s triggers, and effective coping techniques.
This idea of “emotional intelligence” makes me think of the “layers of trauma” or the way that trauma is inserted into our layered consciousnesses. The reason it reminds me about this is because I feel that I often intellectualize my language in order to ignore/defend against feeling any of the emotions behind things. I know that it is a defense mechanism, yet, I often feel powerless in front of it. This has definitely made me realize that I could have a linguistic intelligence that has nothing to do with (or does not correlate with) my emotional intelligence. Talk about feeling fractured!
It is also scary to think about the amount of time it takes for chemicals, drugs to come out of our systems so that we can finally start to understand where we stand in life. Hearing stories from friends about heavy metal deposits found in their blood, or hearing about mood stabilizers found in our tap water makes me wonder if I’ll ever be “sober” in this country, or how long it would take for me to “sober up” in a non-sober country.
Is being sober (at least in a sense where one is not consuming/engaging in any addictive behavior/substance) as possible as attaining “perfection?” The fact that heavy metals can be leaked in the air and that we can be consuming psychotropic medication in our tap water makes me a bit wary of ever hoping to attain a level of detox that will allow me to feel my “true health.”
It’s a definite goal though.
It is fascinating to learn that the brain isn’t ready for significant treatment for at least 1-2 months after full detox. However, it is not surprising that the relapse rate is so high considering just this one piece of evidence and scientific findings. The question of what should the client do in the meantime between detox and actual addiction treatment is an interesting one. Obviously, the client should remain in the residential facility and not be discharged (if the client detoxes in a residential facility). The 1-2 months after full detox could be crucial to the client’s success depending on how that down time is managed. My first thoughts were to be utilizing that time to grow, build and enhance community and especially relations. This support from family and the community is vital to the client’s success. This can be done in several ways, but family therapy comes to mind first. Psychoeducation is another good idea for the client to learn about their addiction, how they can manage it and how they can be successful in life and in managing their addiction. Self discovery would be a good thing for the client to pursue, so that once addiction treatment actually begins they would already have a pocket full of personal insights and behavior.
Edgar, you have brought up a interesting point that I have not consider. Sounds like when you “intellectualize your language” you internalize your emotions. Hmm, it could be that simplicity in our lives has the potential to help us to be more healthy emotionally. Complications and distractions could mask our true feelings and be agents of denial. Your “linguistic intelligence” can actually get in the way of your emotional intelligence. This goes to show that IQ does not necessarily determine success and certainly does not determine whether someone will or will not be prone to addictive behavior. Emotional intelligence seems to be a better indicator of such behavior.
Jennifer, your statement that the clients should utilize the “time to grow, build and enhance community and especially relations,” and your points about learning and self discovery, are major aspects of emotional intelligence. I would also add self-worth, self-respect, and practicing positive coping techniques.
A nice point about intelligence vs emotional development. And it may go beyond that to actual personality. For people may not need as much intelectual stimulation from their partners as they need emotional stimulation.
Thanks.
First of all, I find it obviously necessary to conduct neuropsych tests on patients following detox to determine optimal times to begin treatment. I am surprised this has not been a common practice until now. A person’s brain has to be prepared to benefit from treatment. The answer to what we should do between detox and treatment is definitely a complex one. Obviously, the environment a person is in can play a big part in the possibility of relapse. Ensuring a person is surrounded by family and loved ones that can provide emotional support is imperative. The treatment should certainly be aimed at addressing the patient’s emotional level, rather than their intellect. Smart people make bad choices all the time. Emotionally balanced people stand a better chance to make better decisions. The brain takes times to develop new pathways and therefore patience and perseverance is necessary on the part of the patient and the treatment provider.
Well said.
J
After reading this post I IMMEDIATELY sent it to some people I know who are struggling with trying to help a family member out of addiction and into recovery. This was more than insightful and relavant. Thank you.
Great, thanks!
It is a nice point about intelligence vs. emotional development. But I see that intelligence plays a big role in making different opinions more closely. I believe that intelligence is essential in any successful marriage. I agree that emotional development between couples is important, but it had to be with the same level of intelligence. If there is a big different in intelligence between any two couples, their life will suffer from a lot of problems.
For what person should do between detox and treatment is working. I think working is really important as he will feel that he is an effective person and that his life worth something. By getting involved in work, he will forget his addiction. The person who is working will feel that he should give more efforts to his work.
I am not sure I understand you correctly, but my point is that often individuals in a relationship can have very different IQs, but rarely do they have significantly different emotional or developmental IQs. And you are right, different IQs often do lead to problems in relationships, just as different emotional IQs do. I agree work is important, but it can also be stressful and lead a person right back into their addiction, often because they underlying developmental issues have yet to be addressed. Timing of interventions is critical. Thanks much for your feedback!
J
I found your post to be very insightful! If more drug treatment and rehabilitation centers took the same time and investment in their patients as Dr. Fitzgerald has I feel that the positive outcomes for patients in these programs would be astonishing. I also think it is important to note the significance of establishing the fact that “it’s not intelligence that matters so much as the level of emotional development” not only when working with addicts but in relationships in general. I find it particularly interesting when Dr. Fitzgerald discusses how one it takes for the effects of different kinds of drugs to completely leave the brain and how this directly impacts the effectiveness of treatment for addicts. I think of several people that I know who have been in treatment programs and relapsed shortly after leaving. After reading this blog post I wonder, did the treatment/program fail for my friends because their brain wasn’t ready to be treated? I also wonder what the connection is between TBI patients and drug addicts?
I own a drug testing lab in Virginia and I appreciate the views and information I just read about the critical lessons. It assists me in communicating with the people who come in to be tested and the employers who hire us to do pre-screening and employment screens. A friend of mine has a sister in treatment and this program is 12-18 months long. Afte reading this article I bleieve her chances for success are very good. This is a great place for people like me to come for information.
Thanks for the nice feedback!
J
I find it quite interesting to learn about the natural healing process that takes place in the brain once someone has gone through substance detoxification. I had no idea that it took so long for the brain to heal itself to the point of being capable of learning and processing new information. This completely makes sense though. From what I understand, most rehab environments contain a detox element immediately followed by a rehabilitation treatment plan. Some of these programs are as little as 30 days. I have noticed that the shorter the rehab treatment, the less likelihood for complete recovery-this makes sense. From what we know now, the brain is not capable of processing new information and strategies within the 30 days, or even 60 or 90 days. By the time treatment is over the brain is just getting to the point to where it can completely process the new information being provided. This seems like a waste of time and money. I can only imagine how the patient feels during this time.I hope that with this discovery of how the brain heals itself and the time required to to do so after detoxifying, that current treatment plans can be reassessed and modified to create the best manageable approach with the highest positive outcomes.
While reading your section on emotional intelligence and addiction I was reminded of a familiar scenario. My older brother is one of those really smart people who truly believe he can think himself out of his addiction. He runs himself in circles and as a result runs those who try to help him in circles. With my brother, his situation is further complicated because he also has a high level of emotional intelligence (or at least comes off as he does). Anyone who attempts to have the addictions discussion with him somehow leaves convinced that he does have a grip on reality after all. But the reality of the situation is that I have already seen the emotional intelligence rut that he is in. He is first to agree that he has a problem, but he doesn’t actually talk about his problem. He has lost his ability to go deeper with subjects because his dependence is not allowing him to. It saddens me and it seems as if nothing will ever change for him. He could have done anything that he wanted to do with his life-he is that smart.
Don’t be so sure nothing will ever change for him. Life is a moving target, and sometimes people are exactly where they need to be. Hang in there, continue to discuss addiction with him in a nonjudgmental manner, and he may surprise you :)
J
I was very surprised when I saw that image of the brain with normal function, 10 days after the last abuse, and then 100 days after the last abuse. I had no idea it took that long for your brain to regain regular activity. You didn’t mention how long the cocaine abuser had been doing the drug however. I was curious if that image was from users who had been doing cocaine for a couple years or a couple weeks? Also, will the brain regain normal function quicker for first time users? I would imagine so since it probably wouldn’t be dependent on it yet. It also seems that the bottom half of the brain (in the picture) seem to regain more activity quicker than the top half. I don’t know if that could mean anything, but it could be interesting to look into.
I agree with you that it is best to wait on treatment with a patient who is still detoxifying. It only makes sense. However, the 1-2 month waiting period can be dangerous because the abuser may relapsed if they are not monitored closely.
Thanks for the blog!
Fascinating reading. I am recovering from multiple addictions to alcohol, crack, opiates and, easily the most damaging benzos. I do not fully understand where you are drawing distinctions. Having had habits and recovery periods each drug has very different recovery times. The duration of benzo recovery is well over a year. Opiates, you feel stablish after six months. This is talking from within rather than without. Your point on emotional development is very good. However none of the posts I read differentiated addiction brain recovery types. The rehabs for each drug require completely different approaches. Lumping them in together makes reading all the comments confusing. Understanding of opiate recovery seems to be improving yet it is often the model applied to other drug recovery. I suggest being more specific might help. I struggle to understand when people here are talking about physiological dependence and when they mean habitual behaviour. These are surely treated as separate subjects? Overall reading all this is reassuring in the neurological approach to addiction. I have read some neuropsychology but any suggestions as to what to read specifically on addiction. Thank you
Thanks for the insightful feedback! You make some very good points, and I will think more about how different objects of addiction require at times the same approach, and at other times, different paths. You are right that brain healing is very different for different drugs, so there maybe a better way than lumping all together as you say. That said, most are addicted to a package of behavior, so I am not convinced that it is possible to differentiate addiction brain recovery types. I do think people have different brain elasticity, and brain healing will be variable. We still have a long ways to go in linking out interventions with brain function. In sum, enhancing emotional developmental capacities, at all levels of brain function, is necessary.
J
I have only scratched the surface of emotional development in my psychology course, but your piece allowed me to see how important emotional development is. I knew a couple in a similar situation as the one you talked about. They were going through a divorce and looked for a therapist to help resolve their issues. There was a lot going on within the marriage, but one of the main problems was the level of the wife’s emotional development.
She was traumatic issue when she was at a young age and it stunted her emotional development. She had other various emotional issues that came from her childhood that has greatly impacted her life that she herself did not know of until she searched for professional help. At times she would revert back to that age emotionally, developmentally and psychologically. Her husband was not able to sympathize with her traumatic issue and did not know how to handle it when she would revert back to that stage in her life.
It is amazing to see how emotional development could play such a large role in attraction and relationship building. We as a population focus on measuring IQ, but we overlook EQ.
It makes sense the brain needs time following detoxification to heal before it can absorb and process the information discussed in treatment. I think the time to heal depends on the drug and how long the abuse has been going on for. Its funny how some people believe drug abuse is a choice and not a disease when there is science to back it up that it is a disease. To answer the question about what to do with a person between detox and treatment is a challenging one. After detox you don’t want them to be around anything that can trigger them to relapse yet you don’t want to get them into treatment before their brains are able to benefit from it. I don’t think the patients should be placed back in their previous environment before detox to wait for treatment. There are too many triggers around. I think there should be a program for people who are awaiting treatment should be an option. Though, hopefully insurance would cover the cost or maybe the patients could work for their stay. I think this program should include a safe place for them with the least amount of triggers and a positive environment to keep them progressing. Maybe offer some sort of structure to help support them in their new healthy life style. Some people’s treatments might take longer then others but if these recovering addicts don’t have some sort of structure and a support system to keep them from relapsing before they go to treatment the process of recovering will take much longer.
I think the approach that one needs to help people grow emotionally..”helping those who struggle with addiction developmentally catch-up from the emotional age at which they are stuck” I have never considered emotional development as something that can be taught or learned.
In my own experience, I have a father who is a retired neurosurgeon. It goes without saying that he is smart beyond belief, and VERY cerebral. However, he is as emotionally mature as a pre-pubescent. It’s really sad actually. He gets so attached to his beliefs and views that it becomes nearly impossible for him to carry on an intelligent debate or even a conversation without some sort of defensive stance being taken. Is emotional intelligence something that can be learned? I say yes, but just knowing about something doesn’t mean that you KNOW IT, or know how to do it.
This quote:
“There are some really smart people that get caught up in addiction, and often they can be among the hardest to treat because they believe they can think their way out of the problem. But you cannot “think” your way to a higher level of emotional functioning.”
Sums it up. How does one learn how to function on a higher emotional level?
Thanks for your comment about development. The short answer is that we can absolutely help people developmentally catch-up, increase their emotional IQ, and engage more deeply in the world. But it takes time, and a person has to have motivation for gain the developmental capacities, which of course means they must see how their developmental blindspots are hurting them. For more information on this topic, read Growth of the Mind by Stanley Greenspan, then read his more clinical book: Developmentally Based Psychotherapy. Also, check out: http://addictionmanagement.org/2009/07/autism-expert-can-help-those-who-struggle-with-addiction/ and http://www.childtrauma.org/images/stories/Articles/neurosequentialmodel_06.pdf
Best
J
Great article, John. Really opened my eyes to the amount of time addicts need to spend in treatment. My uncle recently went through a rough time with crack cocaine and heroin and I am SURE that if he spent more than a month in treatment, he would not have relapsed like he did. Although sober, he was still damaged, broken, and weak after leaving treatment. There must be ways that we can create additional funding to prolong the time that addicts stay in treatment. Perhaps a minor minor tax increase? I don’t know much about finances but it seems like if everyone chipped in a couple pennies every year, our facilities would have enough money to house addicts for months at a time.
Thanks Jacob. Our system needs revamping, and those who struggle like your uncle need to have access to long term care far beyond 30 days. One approach if funds are limited, is to forgo residential treatment and use the money over a longer period of time to pay for outpatient which studies suggest is equally as effective.
J
The story about the wife and husband shocked me at first. This is because I have always believed that I wanted to marry some one with similar intelligence levels. I understand that emotion levels are a huge part of marriage and probably why they lasted as long as they did. Could the intelligence be part of the reason they are getting divorced? Did they stay married because of kids? These are reasons why I think somewhat intelligence level is on the same level as emotional level.
Please may I ask sir, where are your citations for so many points you put forward?
Or at least a reference list would suffice.
I am not disagreeing and I understand the importance of presentation with such a website.
If you could contact me regarding any possible sources for lots of well worded ideas you have presented, specifically regarding neuroimaging and how neuroscience has impacted the field of rehabilitation that would be brilliant.
The post is based off of my three years of working for two neuropsychologists, and my observations during that time. But there are plenty of peer-reviewed journal articles on this topic supporting my post. You are free to contact by email off the site if your own lit search does not turn up anything.
J
I don’t think intelligence can hold attractiveness in a long term without compatibility or emotional bond. When it comes to relationship, I have always questioned why researchers based their study on intelligence instead of the heart or emotional intelligence. Indeed, the lack of emotional intelligence measurement methods reflects our choice of approach. Personally, I suggest we have different means of measuring emotion. The comment of smart people is harder to treat reminds me of a motivational psychology class. We discussed how some students are told to work harder and another group are told they’re doing great. Overconfidence have negative impact on performance, this explains why the student group who are told to work harder have better performance in a long run. Similarly, I think it partly explains why an intellectual person is healed slowly. On the other hand, I wonder how emotional intelligence and micro-expression, the work of Dr. Paul Ekman are related and how logical intelligence helps us improve emotional intelligence. Everyone is different as well as his or her learning style and time of treatment. Neuroplasticity gives us a general time frame of treatment for age group. I wish the research on cocaine contained age data. However, spending inadequate time in treatment is wasting money. Saving becomes vain. At the end, I’m touched by how researchers take care of their patients, such meticulous researchers.
I don’t think intelligence can hold attractiveness in a long term without compatibility or emotional bond. When it comes to relationship, I have always questioned why researchers based their study on intelligence instead of the heart or emotional intelligence. Indeed, the lack of emotional intelligence measurement methods reflects our choice of approach. Personally, I suggest we have different means of measuring emotion. The comment of smart people is harder to treat reminds me of a motivational psychology class. We discussed how some students are told to work harder and another group are told they’re doing great. Overconfidence have negative impact on performance, this explains why the student group who are told to work harder have better performance in a long run. Similarly, I think it partly explains why an intellectual person is healed slowly. On the other hand, I wonder how emotional intelligence and micro-expression, the work of Dr. Paul Ekman are related and how logical intelligence helps us improve emotional intelligence. Everyone is different as well as his or her learning style and time of treatment. Neuroplasticity gives us a general time frame of treatment for age group. I wish the research on cocaine contained age data. However, spending inadequate time in treatment is wasting money. Saving becomes vain.I’m touched by how researchers take care of their patients, such meticulous researchers.
I’m really in awe about your first lesson. I was always taught that intelligence is what gets you through things, but it makes sense now that I think about it that emotional development is more important. I really like how you put it, “You cannot think your way to a higher level of emotional functioning.”
I’m also really surprised and sad to hear about the lapse time between detox and treatment. Letting the person out of detox and into the open world is going to cause a lot of triggers or reminds of the drugs and more than likely cause relapse. Which means the individual has to start all over again. I’m not 100% sure what is all involved in drug treatment, but maybe in the month or two proceeding detox, there could be another program set-up to help not only motivate the person to stay away from drugs, but possibly help them set up a life for them to go back to when they are done with treatment?
Thanks for the nice feedback!
J
I really appreciated your article!
It made me think about how important it is that when we think about addiction, we focus on the person with the disease and what will work to help them, rather what would make us feel better. For example, you wrote about the fact that addiction program are most effective after being clean for a month. While this may be best for the addicted, it would be hard to the family and friends to expect that they cant help their loved one right away. Or it is easy to treat those who have suffered with TBIs like anyone else, because it is faster and ‘easier.’ However, like you said, it is important to meet those with TBIs where they are and work with them in ways that work specifically for them.
Thanks for the reminder in empathy! And for the new information on effective addiction treatments.